Understanding Coronary Artery Disease: Causes, Prevention, and Global Health Impact
This article explores coronary artery disease (CAD), the leading cause of death worldwide. It covers the causes, risk factors, symptoms, diagnosis, and treatment options for CAD. The article emphasizes the importance of lifestyle changes, such as a healthy diet, regular exercise, and smoking cessation, in preventing the disease. It also highlights the global burden of CAD and the need for public health initiatives and policies to reduce its impact.
INDC Network : Health : Determining the disease that affects humans the most can be complex, as it can be assessed from various perspectives, including prevalence, mortality, morbidity, or societal impact. However, cardiovascular diseases (CVDs), particularly coronary artery disease (CAD), are the leading cause of death globally and can be considered among the most impactful diseases affecting humans.
This essay delves into the nature of cardiovascular diseases, particularly coronary artery disease, discussing its causes, prevention, and the broader implications for global health.
Introduction to Cardiovascular Diseases
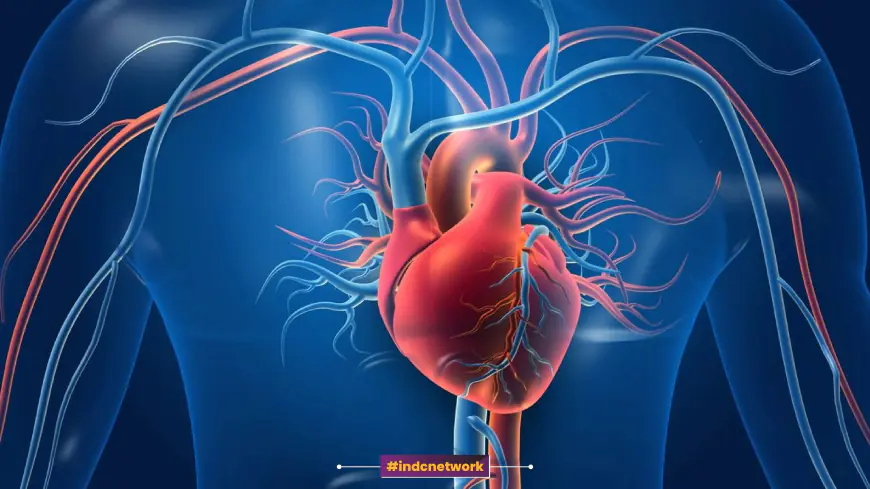
Cardiovascular diseases encompass a group of disorders of the heart and blood vessels, including coronary artery disease, cerebrovascular disease (like stroke), peripheral arterial disease, rheumatic heart disease, congenital heart disease, deep vein thrombosis, and pulmonary embolism. Among these, coronary artery disease stands out as the most significant due to its high prevalence and contribution to mortality.
According to the World Health Organization (WHO), CVDs are the number one cause of death globally, responsible for an estimated 17.9 million deaths each year, which is about 31% of all deaths worldwide. Of these, 85% are due to heart attack and stroke.
Understanding Coronary Artery Disease (CAD)
1. What is Coronary Artery Disease?
Coronary artery disease (CAD) is a condition where the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to the buildup of cholesterol and other materials, collectively known as plaque, on their inner walls. This process is called atherosclerosis. As the plaque builds up, the arteries narrow, reducing blood flow to the heart muscle. This can lead to symptoms like chest pain (angina), shortness of breath, and other symptoms. If a plaque ruptures, it can cause a blood clot that blocks blood flow, potentially leading to a heart attack.
2. Risk Factors for Coronary Artery Disease
The development of CAD is influenced by a combination of risk factors, including:
-
High Blood Pressure (Hypertension): This condition increases the heart's workload, causing the heart to thicken and become stiffer, which can lead to coronary artery disease.
-
High Blood Cholesterol Levels: High levels of low-density lipoprotein (LDL) cholesterol, often referred to as "bad" cholesterol, contribute to plaque buildup in the arteries.
-
Smoking: Tobacco smoke damages the blood vessels and increases the risk of atherosclerosis. Smokers are at a much higher risk of developing CAD compared to non-smokers.
-
Diabetes: Diabetes significantly increases the risk of CAD, as high blood sugar levels can damage blood vessels over time.
-
Obesity: Excess body weight, especially around the abdomen, is associated with high blood pressure, high cholesterol, and an increased risk of CAD.
-
Physical Inactivity: Lack of regular physical activity contributes to obesity and increases the risk of CAD. Regular exercise is important for maintaining heart health.
-
Unhealthy Diet: Diets high in saturated fats, trans fats, cholesterol, salt, and sugar can contribute to the development of CAD. Conversely, a diet rich in fruits, vegetables, and whole grains can reduce the risk.
-
Excessive Alcohol Consumption: Drinking too much alcohol can raise blood pressure, contribute to obesity, and lead to heart failure.
-
Family History: A family history of heart disease increases the risk of CAD, especially if a parent or sibling developed heart disease at an early age.
-
Age: The risk of CAD increases with age. Men aged 45 or older and women aged 55 or older are at higher risk.
-
Stress: Chronic stress may contribute to an increase in heart disease risk by raising blood pressure and contributing to other risk factors such as smoking, overeating, and lack of physical activity.
-
Gender: Men are generally at higher risk for CAD at a younger age than women. However, after menopause, a woman’s risk increases and can equal that of men.
3. Pathophysiology of Coronary Artery Disease
The pathophysiology of CAD involves the gradual accumulation of atheromatous plaques in the coronary arteries. The process can be broken down into several stages:
-
Endothelial Dysfunction: The initial stage of CAD involves damage to the endothelium, the inner lining of the blood vessels. This damage can be caused by high blood pressure, smoking, or high cholesterol levels. Once the endothelium is damaged, cholesterol and other substances begin to accumulate at the site of injury.
-
Formation of Fatty Streaks: Over time, these accumulations form fatty streaks, which are the early signs of atherosclerosis. These streaks are composed of lipid-laden cells called foam cells, which are derived from macrophages that have engulfed LDL cholesterol.
-
Plaque Formation: As fatty streaks grow, they become more complex and form plaques. These plaques consist of a lipid core surrounded by a fibrous cap. Over time, the plaques can become calcified, further narrowing the arteries and reducing blood flow to the heart muscle.
-
Plaque Rupture and Thrombosis: In some cases, the fibrous cap of a plaque can rupture, exposing the lipid core to the bloodstream. This triggers the formation of a blood clot (thrombus) at the site of the rupture. If the clot becomes large enough, it can completely block the coronary artery, leading to a heart attack.
Clinical Manifestations of Coronary Artery Disease
The symptoms of CAD can vary depending on the severity of the disease and the extent of arterial blockage. Some people may be asymptomatic, while others may experience the following symptoms:
-
Angina: Angina is the most common symptom of CAD. It is characterized by chest pain or discomfort, often described as a squeezing, pressure, heaviness, or tightness in the chest. Angina can be stable (occurring with exertion and relieved by rest) or unstable (occurring at rest or with minimal exertion and not relieved by rest).
-
Shortness of Breath: Reduced blood flow to the heart can cause shortness of breath, especially during physical activity.
-
Fatigue: Chronic fatigue or a feeling of being tired all the time can be a symptom of CAD, particularly in women.
-
Heart Attack (Myocardial Infarction): A heart attack occurs when a plaque ruptures and a blood clot forms, blocking blood flow to a part of the heart muscle. Symptoms of a heart attack may include severe chest pain, shortness of breath, nausea, vomiting, sweating, and loss of consciousness. A heart attack is a medical emergency and requires immediate treatment.
-
Arrhythmias: CAD can lead to irregular heartbeats or arrhythmias, which can cause palpitations, dizziness, or fainting.
Diagnosis of Coronary Artery Disease
Diagnosing CAD involves a combination of medical history, physical examination, and various diagnostic tests, including:
-
Electrocardiogram (ECG): An ECG records the electrical activity of the heart and can detect abnormalities that may indicate CAD or a previous heart attack.
-
Stress Test: A stress test evaluates how the heart performs under physical stress, usually by walking on a treadmill or riding a stationary bike while being monitored by an ECG.
-
Echocardiogram: An echocardiogram uses ultrasound to create images of the heart, allowing doctors to assess the heart's function and structure.
-
Coronary Angiography: Coronary angiography is an invasive procedure in which a contrast dye is injected into the coronary arteries, and X-rays are taken to visualize the blood flow and detect blockages.
-
Cardiac CT or MRI: These imaging tests provide detailed images of the heart and can help in assessing the severity of CAD.
Treatment of Coronary Artery Disease
The treatment of CAD aims to relieve symptoms, slow the progression of the disease, and reduce the risk of complications such as heart attack. Treatment options include lifestyle changes, medications, and medical procedures.
1. Lifestyle Modifications
-
Dietary Changes: A heart-healthy diet is crucial in managing CAD. This includes reducing the intake of saturated fats, trans fats, cholesterol, and salt, while increasing the consumption of fruits, vegetables, whole grains, and lean proteins. The Mediterranean diet, which emphasizes healthy fats like olive oil and includes plenty of fish, fruits, and vegetables, has been shown to reduce the risk of heart disease.
-
Exercise: Regular physical activity helps maintain a healthy weight, lowers blood pressure, improves cholesterol levels, and reduces the risk of CAD. The American Heart Association recommends at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity exercise each week.
-
Smoking Cessation: Quitting smoking is one of the most effective ways to reduce the risk of CAD and improve overall heart health. Smoking cessation programs, nicotine replacement therapy, and medications can help people quit smoking.
-
Weight Management: Achieving and maintaining a healthy weight can reduce the risk of CAD. This involves a combination of a healthy diet and regular exercise.
-
Stress Management: Managing stress through relaxation techniques, mindfulness, yoga, or counseling can help reduce the risk of CAD.
2. Medications
Several medications are available to treat CAD and its associated risk factors. These include:
-
Antiplatelet Drugs: Medications like aspirin and clopidogrel help prevent blood clots from forming by making the blood less likely to clot.
-
Statins: Statins are used to lower LDL cholesterol levels, reducing the risk of plaque formation and progression of atherosclerosis.
-
Beta-Blockers: Beta-blockers help reduce blood pressure and heart rate, reducing the heart's workload and the demand for oxygen.
-
ACE Inhibitors and ARBs: These medications help lower blood pressure and reduce the risk of heart failure in people with CAD.
-
Calcium Channel Blockers: These drugs relax and widen the blood vessels, improving blood flow to the heart and reducing chest pain.
-
Nitrates: Nitrates, such as nitroglycerin, are used to relieve angina by relaxing the blood vessels and increasing blood flow to the heart.
-
Diuretics: Diuretics help lower blood pressure by removing excess fluid and salt from the body.
3. Medical Procedures
In some cases, medical procedures may be necessary to treat CAD:
-
Angioplasty and Stenting: Angioplasty is a procedure in which a balloon is inserted into a narrowed or blocked coronary artery and inflated to widen the artery. A stent, a small mesh tube, is often placed in the artery to keep it open and maintain blood flow.
-
Coronary Artery Bypass Grafting (CABG): CABG is a surgical procedure in which a blood vessel from another part of the body, such as the leg or chest, is used to create a bypass around the blocked or narrowed coronary artery, restoring blood flow to the heart muscle.
-
Enhanced External Counterpulsation (EECP): EECP is a non-invasive procedure that can improve blood flow to the heart by inflating and deflating cuffs around the legs and lower body, helping to open small blood vessels and promote the development of new blood vessels.
Prevention of Coronary Artery Disease
Preventing CAD involves addressing the modifiable risk factors and making lifestyle changes that promote heart health. Key preventive measures include:
1. Healthy Diet
A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats is essential for preventing CAD. Limiting the intake of saturated fats, trans fats, cholesterol, and salt can help reduce the risk of atherosclerosis and high blood pressure. Incorporating foods high in omega-3 fatty acids, such as fish, nuts, and seeds, can also support heart health.
2. Regular Physical Activity
Engaging in regular physical activity helps maintain a healthy weight, lower blood pressure, improve cholesterol levels, and reduce the risk of CAD. A combination of aerobic exercises, such as walking, jogging, swimming, or cycling, along with strength training exercises, can provide comprehensive benefits for heart health.
3. Smoking Cessation
Smoking is a major risk factor for CAD, and quitting smoking is one of the most effective ways to prevent the disease. Smokers who quit can significantly reduce their risk of CAD and improve their overall health.
4. Weight Management
Maintaining a healthy weight through a combination of diet and exercise is crucial for preventing CAD. Obesity is associated with several risk factors for CAD, including high blood pressure, high cholesterol, and diabetes.
5. Blood Pressure Control
High blood pressure is a significant risk factor for CAD, and controlling blood pressure through lifestyle changes and medications can reduce the risk of heart disease. Regular monitoring of blood pressure and adherence to treatment plans are important for maintaining healthy blood pressure levels.
6. Cholesterol Management
Managing cholesterol levels through a heart-healthy diet, regular exercise, and medications can help prevent the development of atherosclerosis and CAD. Regular cholesterol screenings and adherence to treatment plans are essential for managing cholesterol levels.
7. Diabetes Management
People with diabetes are at a higher risk of developing CAD, and effective management of blood sugar levels through diet, exercise, and medications is crucial for reducing this risk.
8. Stress Management
Chronic stress can contribute to the development of CAD by raising blood pressure and promoting unhealthy behaviors such as smoking and overeating. Managing stress through relaxation techniques, mindfulness, and counseling can help reduce the risk of CAD.
9. Regular Health Checkups
Regular health checkups and screenings for blood pressure, cholesterol levels, and blood sugar levels can help detect risk factors for CAD early and allow for timely intervention.
The Global Burden of Coronary Artery Disease
The global burden of CAD is immense, with the disease contributing to a significant proportion of deaths and disability worldwide. According to the WHO, low- and middle-income countries are disproportionately affected, accounting for over 75% of CVD-related deaths. The economic impact of CAD is also substantial, with the cost of healthcare, lost productivity, and long-term disability placing a significant burden on individuals, families, and healthcare systems.
Efforts to reduce the global burden of CAD require a comprehensive approach that includes public health initiatives, access to healthcare, education, and policies that promote heart-healthy behaviors. Addressing the social determinants of health, such as access to nutritious food, safe environments for physical activity, and affordable healthcare, is essential for reducing the prevalence of CAD and improving overall health outcomes.
Conclusion : Coronary artery disease is a major public health concern, affecting millions of people worldwide and contributing to a significant proportion of deaths and disability. The disease is largely preventable through lifestyle changes, including a heart-healthy diet, regular physical activity, smoking cessation, and stress management. Early detection and management of risk factors such as high blood pressure, high cholesterol, and diabetes are crucial for preventing the development and progression of CAD.
Addressing the global burden of CAD requires a comprehensive approach that includes public health initiatives, access to healthcare, and policies that promote heart-healthy behaviors. By adopting these strategies, individuals can reduce their risk of CAD and improve their overall health, while healthcare systems and policymakers can work towards reducing the prevalence and impact of this life-threatening disease.